Retinopathy of prematurity is the cause of anxiety for families of micro-preemies and extremely premature babies. They fear that this condition may lead to vision problems or blindness after discharge home.
ROP stands for Retinopathy of Prematurity and is a disease of growing and proliferating blood vessels in the back of immature eyes. Premature babies are always born with immature eyes. During the first months after birth, blood vessels in their eyes must grow and multiply. Disruption of that natural process by injuring factors may lead to ROP.
The most severe forms of ROP may result in complete blindness; hence physicians and parents have to pay attention to this problem. Ophthalmologists will tell you that ROP is one of the significant causes of blindness in the USA.
Eye anatomy
Before we go any further on the topic of ROP, let me review some general information regarding eye anatomy. If you have some knowledge about the structure and functioning of the eye, just go directly to the next section of my article.
In the picture below, you can see the eye that is cross-cut along its anterior-posterior axis.
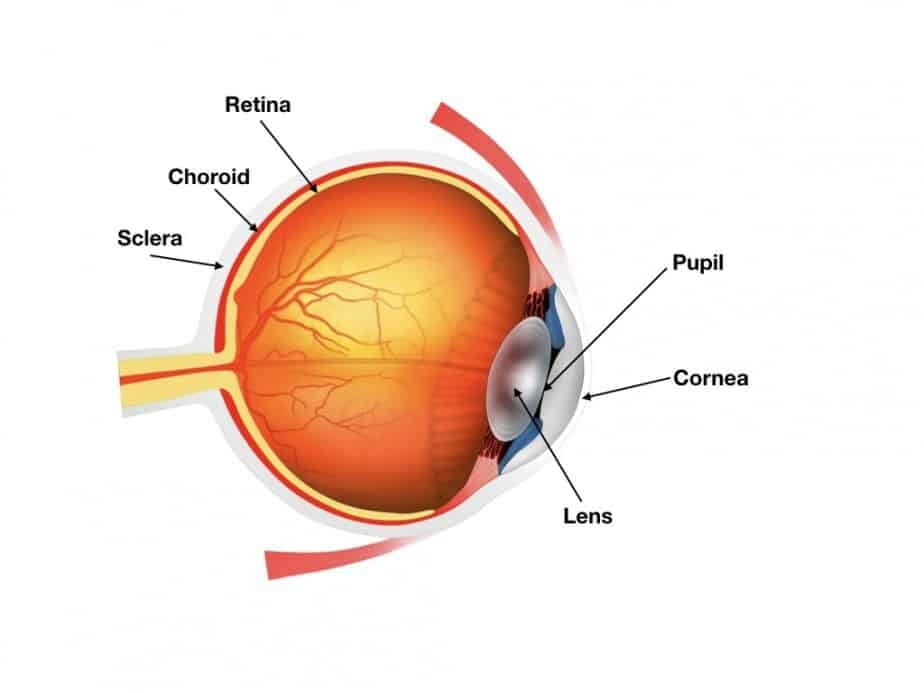
An eye is a globular structure covered by several membranes and filled with a liquid substance called virtuous humor.
Cornea – is a clear and transparent dome-like structure covering the front of the eye.
Iris – is a thin, colored, and circular structure that controls the size of the pupil and is located behind the cornea and in front of the lens.
Pupil – is a round opening within the iris that allows light to go inside the eye.
Lens – is a transparent structure located behind the iris capable of bending or focusing light rays on the back of the eye where vision receptors are located.
Vitreous humor – is a fluid that fills eye globe between lens and retina.
Retina – is an internal lining of the eye filled with light-sensitive receptors. These receptors get stimulated by light and produce electric signals that are sent through the optic nerve to brain areas responsible for vision.
Choroid – is a membrane that lies behind retina and supplies nutrition to the eye through blood vessels.
Now, when we look through the pupil inside the eye, we can see the back of the eye. We obtain such a view during a fundoscopic exam that eye doctors perform after dilating the pupils. I want you to pay great attention to this view because the staging and severity of ROP will be based on this view.
In this view, we see optic disc located a little off-center towards the nasal part of the retina. An optical disc is a place where the optic nerve enters the eye. Remember that the optic nerve conducts visual electric impulses between the eye and brain.
A macula is located laterally to the optic disc. It is is a place with a maximum concentration of visual receptors. The fundus is covered with a pinkish internal lining called the retina. On the bottom of the eye, we can also see numerous blood vessels spreading from the optic disc area towards the periphery of the eye.
Blood vessels in premature babies are not fully developed yet. They start growing from the center at around 15 – 18 weeks of gestational age, and their growth ends only at 36-40 weeks of GA. During that period of eye maturation, various factors may disturb vascular growth and lead to Retinopathy of Prematurity – ROP (Source).
How common is Retinopathy of Prematurity (ROP)
ROP occurs more frequently in the tiniest and most premature babies. Let’s look at the table below to see its incidence:
| Age at birth: | All ROP | Severe ROP |
|---|---|---|
| <24 weeks | 95% | 18% |
| 25 weeks | 92% | 12% |
| 26 weeks | 85% | 12% |
| 27 weeks | 72% | 5% |
| 28 weeks | 66% | 4% |
You can notice right away that the more premature baby is, she/he is at higher risk to have ROP. For example, more than 90% of babies born at 25 weeks or less will develop any kind of ROP, and more than 10% of them will have a severe form of it.
At 28 weeks of gestation age, those numbers drop to 66% for any ROP and to 4%. for severe ROP.
Which babies develop ROP?
Risk factors associated with ROP:
- Low birth weight
- Low gestational age at birth (Particularly below 28 weeks)
- Unmonitored oxygen use
- Hyperglycemia needing insulin treatment
We also know that if the baby requires more aggressive treatments or develops complications in NICU, such a baby will have a higher risk for ROP.
From epidemiological studies, we know that babies who stay for a long time on a ventilator, have abnormal blood gases, require blood transfusion or develop infections, pneumothorax, or intraventricular hemorrhages have a much higher chance to have ROP.
(Pneumothorax is a condition in which portion of the lung ruptures and air leaks out of the lung and gathers in the chest and subsequently compresses the lung preventing it from expanding).
(Intraventricular hemorrhage is a bleeding in one of the areas in the brain to which very premature babies are prone).
Unmonitored exposure to high oxygen concentrations during the first weeks of life also is associated with a higher incidence of ROP. Unfortunately, it is still unclear to us what is the optimal way of providing oxygen to babies. It appears that lower oxygenation targets are safer for the eyes. On the other hand, we know that lower oxygen levels, particularly in the smallest babies, increase the number of deaths.
At this time, most NICUs are targeting oxygen saturations in the range of 90%-95%. Only a few doctors advocate targeting oxygen saturations below 85% due to increased mortality in tiniest babies. Please remember that these numbers may change at any time as new data get published.
(Oxygen saturation is a number obtained from the monitoring devices that allow us to assess oxygen levels in a baby).
Mechanism of ROP
ROP may develop in 2 phases. Phase 1 starts soon after birth and is defined by the arrest of blood vessels growth due to exposure to too much oxygen. The term “too much” should be understood as it is too much for growing blood vessels on the bottom of the eye, but often the same amount of oxygen is appropriate and even necessary for that baby to live and survive.
I don’t want anybody to think that a baby develops ROP because doctors gave too much oxygen to a baby.
In phase 1, oxygen leads to decreased production of so-called blood vessels growth factors (Erythropoietin and VEGF) and that in turn leads to the arrest of blood vessels growth.
Phase 1 may evolve into Phase 2, and that usually occurs after 32 weeks of corrected gestational age.
In Phase 2, due to poorly developed blood vessels, the retina is starved of oxygen. That situation stimulates over-production of growth factors and unhealthy retinal blood vessels growth, resulting – in the worse scenario – in retinal detachment and blindness.
In many premature babies, retina revascularizes almost normally after phase 1, and retinal detachment does not occur. However, many babies, even with mild ROP, may end up with insufficient numbers of photoreceptors (light receptors) in their eyes and will develop various vision problems.
Which premature babies should be screened for ROP?
What are the criteria for ROP screening in preemies?
To diagnose ROP disease early and be able to start treatment to limit the negative consequences of the disease, we must screen babies for ROP.
Many professional organizations stated that all babies born at less than 30 weeks of GA or with a birth weight of fewer than 1500 grams should be regularly screened for ROP. Of course, these criteria mean that ALL micro-preemies and extremely premature babies must be screened.
Most of the time, ROP screening is conducted by ophthalmologists in person. In some centers, it is done by technicians who are using special cameras to take pictures of the baby’s eyes and send those to an eye doctor for a reading.
The latter approach is less desirable as it can miss some milder forms of ROP. However, due to a shortage of available eye doctors, it may be the only option to conduct an ROP examination in the hospital where your baby is cared for.
At what age ROP exam should be done?
Screening exams for ROP are not needed until several weeks after birth. You have to remember that a baby is never born with ROP. The baby develops ROP over time.
Based on historical statistical information, doctors decided that ROP exams should start at 30 weeks of corrected gestational age for babies who were born between 22 – 26 weeks and at four weeks after birth for babies born at 27 weeks of GA or more.
Just be aware that individual hospitals may have a little different schedule and policy for those exams.
How is the ROP exam conducted?
The ROP exam is usually conducted at the bedside. In preparation for the exam, eye drops are instilled to dilate the pupils, and sucrose can be given to the baby to make him or her more comfortable. An assistant will swaddle the baby and hold the baby’s head down while ophthalmologist will be looking into the baby’s eyes using special lenses and lights.
The whole exam does not take very long, probably 5-10 minutes, and most babies tolerate it well.
Assessing the severity of Retinopathy of Prematurity
After conducting the ROP exam, the ophthalmologist will assess the severity of illness individually for each eye using four descriptors: zone, stage, the extent of disease, and presence or absence of plus disease.
Let me explain these four terms for you.
The zone is an area of the eye where abnormal blood vessels are found. Zone 1 is the most posterior and of utmost importance because it covers the highest concentration of light receptors. Disease in zone 1 places you at the highest risk for visual acuity loss. ROP in zones 2 and 3 is less dangerous for vision loss.

Based on how the blood vessels and retina look during the exam, the ophthalmologist may classify ROP disease as stage 1-5. Stage 1 being the most benign and stage 5 signifying the most severe form of ROP consistent with retinal detachment.
The extent of the disease is recorded by comparing the bottom of the eye to a clock and by stating how many clock hours are involved. For example, a doctor may say that ROP is present in the left eye from 1 to 4 and then from 7 to 9 clock hours.
Plus disease is present when we see tortuous blood vessels in the retina. ROP with abnormal tortuous vessels is always a more aggressive form of ROP and indicates a high risk of progression towards retinal detachment.
Treatment of Retinopathy of Prematurity
Indications to treat ROP in newborn babies:
- Any stage ROP with the plus disease in zone I
- Stage 3 ROP without the plus disease in zone I
- Stage 2 or 3 ROP with the plus disease in zone II
You may ask why we should treat ROP if we know that the natural evolution of this disease is that it regresses, and current treatments are not the cure for this disease.
It is an excellent question. The answer is that, when we use indications for treating ROP that I listed above, there is less chance for adverse visual outcomes than if we do not treat it at all.
How can we treat severe ROP disease?
Currently, there are options available for the treatment of severe ROP. The first one is laser surgery, also called laser photocoagulation. And the second option is the intravitreal injection of an anti-VEGF agent such as Bevacizumab or Ranibizumab.
These two medications are also used in adults for the treatment of cancer. Their mechanism of action is such that they stop the development of new blood vessels in a tumor and starve it of oxygen. They work similarly in babies, as you may remember, when I talked about aggressive forms of ROP, I explained that they are characterized by the fast growth of abnormal tortuous blood vessels. Those two medications injected locally into the eyes are capable of stopping that abnormal growth in babies.
No large trials exist that would allow us to compare these two treatment options. Both have advantages and disadvantages. It is a good idea to have your baby treated in a center where both options are offered so that the best solution can be chosen.
While deciding which treatment option to use, physicians and parents should take into account various factors.
One of them is the severity of the disease and doctor’s experience and comfort with each technique.
Laser therapy is a long-established therapy, while anti-VEGF treatment is a newer technique, and we have less data on its efficacy and long term visual and systemic outcomes. By systemic consequences, I mean potential effects on the baby’s brain or other organs even though the medication is injected only locally into the baby’s eyes.
The timing of the response after treatment will vary as well. ROP involution will most likely be faster after anti-VEGF therapy than after laser surgery.
We should also think about the burden for the baby – can baby tolerate treatment well? Intravitreal administration of anti-VEGF agents can be done quickly and only with local topical anesthesia at the bedside.
On the other hand, laser treatment will require much more time, will be more stressful for the baby, and will necessitate administration of general anesthesia.
Long term vision outcomes may differ after each therapy; however, that has not been very well documented yet. The risk of myopia or shortsightedness appears to be lesser with anti-VEGF treatment. It also speculated that anti-VEGF therapy might limit permanent peripheral visual field loss.
Prognosis and outcomes for preemies with the diagnosis of ROP
Children with a history of ROP (regardless if they required treatment or not) are at increased risk for the development of myopia, astigmatism, and lazy eye, therefore, they should be undergoing regular check-ups by eye-doctor during their childhood.
It has been determined that long term visual impairment occurs in 7-15% of children with moderate to severe ROP. The risk for an unfavorable visual outcome is highest for babies with ROP stage 3 or higher and ROP in zone 1.
The ROP disease is often a more global indicator of severe complications that the baby was going through during the NICU stay. Severe ROP is a predictor of non-visual functional outcomes. In one study of 1500 babies born with BW below 1250 gm, it was found that 40% of babies with severe ROP had at least one non-visual disability compared with only 16% of babies without severe ROP (Source). Motor developmental delays, cognitive impairments, and a hearing loss were 3-4 times more likely to occur in children with a history of severe ROP than in children without it.
What questions to ask your neonatologist or eye-doctor if you have a premature baby in NICU?
- Is my baby at risk for ROP?
- If yes, when will be the first ROP exam done?
If your baby already has the ROP diagnosis, ask these questions:
- How severe is retinopathy of prematurity in my baby?
- When will be the next ROP exam?
- Does my baby need treatment for ROP, or is it likely to need treatment in the near future?
- Do you provide both options for the treatment of ROP in your hospital? (Laser and medical treatment)
- What is the long term prognosis regarding my baby’s vision?
Summary
In summary, I want to emphasize that ROP is a disease that affects the majority of micro-preemies and extremely premature babies. Newborn babies are not born with this disease; they develop it over time during their hospitalization.
The best approach to it, to prevent devastating outcomes such as loss of vision, is to be very vigilant and start ROP screening exams at appropriate times and institute timely treatment when it is indicated. After discharge home, children who had ROP will need regular follow up to monitor their eye health.
If you have a premature baby born before 32 weeks receiving treatment in the NICU right now, I encourage you to explore my book “Babies Born Early“
Here you can find my other article reviewing all problems that premature babies may develop after birth.
Disclaimer:
This article is only for general information purposes. It should not be viewed as any medical advice. There is a chance that information here may be inaccurate. It would be best if you always discussed all health-related matters with your doctor before making any decisions that may affect your health or health of your family members.

