This article focuses on RSV infections in current and former premature babies. RSV is a virus feared by all parents of premature babies, particularly micro-preemies and extremely premature babies.
As a result of infection with RSV, infected babies may develop severe bronchiolitis and may end up being admitted again to the hospital, and even worse, to the intensive care unit.
What is RSV?
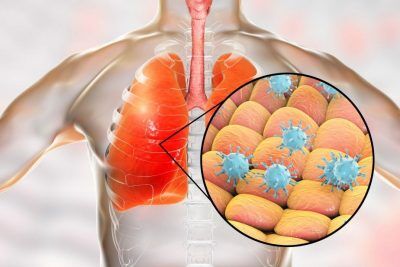
RSV stands for Respiratory Syncytial Virus. It is a virus attacking the respiratory system, specifically upper and lower airways.
You can contract RSV infection by inhaling droplets from the air if you are in the proximity to a sick patient or by direct contact with viruses; for example, touching contaminated surfaces and transferring those secretions to your nasal cavity or your eyes. It seems that if one is not very careful with hand hygiene, it is very easy to get infected.
Who can be affected by RSV infection?
Respiratory Syncytial Virus affects people of all ages but is most dangerous for infants, especially for former micro-preemies and very premature babies. In those babies, it is more likely to lead to severe apnea and pneumonia. (Apnea is defined as pauses in breathing rate or breathing pattern). Pneumonia is defined as an infection in the lungs).
It is worth mentioning that up to 3% of all infants before turning 12 months of age may need hospitalization due to lower respiratory tract infection caused by RSV. Fortunately, most babies who were previously healthy do well and stay in the hospital for no more than 2-3 days.
Sadly, about 100 babies per year will have died each year due to this disease. RSV infection is so common that by 24 months of age, almost all children get that infection at least once.
What are the symptoms of RSV?
Pretty much all affected pediatric patients will have decreased activity, poor appetite, or difficulties with feedings. They will also have a runny nose with a lot of secretions and possibly low-grade fevers.
In infants with the involvement of the lower respiratory airways, we will often see nasal flaring, grunting (making noise while exhaling air), retraction, and need for additional oxygen while breathing.
Those latter symptoms can also be described as increased work of breathing due to airways being plugged by secretions. Secretions lead to increased resistance in the airways making baby work hard when trying to inhale and exhale the air.
How do we diagnose Respiratory Syncytial Virus infection?
The diagnosis of RSV is relatively straightforward. If we get a pediatric patient, especially an infant presenting with respiratory symptoms without a previous diagnosis of asthma during RSV season (October-March), we should suspect RSV infection. To confirm the diagnosis, we can do a nasal swab for secretions and perform so-called RSV rapid antigen testing or send that sample for RSV culture.
Rapid antigen testing will yield results within an hour. RSV culture will take several days to come back. In most cases confirming RSV infection is not that crucial since we do not have specific treatments for RSV infection.
Often, it is more important to rule out other more dangerous conditions, for example, bacterial infections. If bacterial infections are not recognized quickly, they can lead to sepsis (overwhelming infection of the whole body) and even death of the patient.
How do we treat RSV infections?
There is no specific treatment for Respiratory Syncytial Virus infections that is routinely used. The treatment of RSV is supportive. What does that mean? We will be supporting patients’ symptoms, trying to alleviate their severity.
If the baby has a fever, we will give anti-fever medications. If the baby is not able to eat due to poor appetite or nasal secretions, we can feed baby using NG tube or start IV fluids. If the baby has consistently low oxygen levels, we can provide supplementary oxygen for breathing.
If the baby has secretions, we can suction them frequently to ease breathing. In rare situations, if a patient has severely compromised respiratory function, we put such a patient on a ventilator.

For infants with mild to moderate respiratory symptoms, nebulizations with 3% sodium chloride might be helpful (See picture to the left).
The following medications are not helpful in routine treatment of RSV infections:
- Albuterol treatment
- Steroids
- Nebulized epinephrine
- Ribavirin
- RSV immunoglobulins as a treatment
- Routine antibiotics without evidence of bacterial infection
Despite a lack of evidence for the efficacy of the agents mentioned above, some providers still try using them on some patients.
Can we prevent RSV infections?
We can prevent RSV infections by eliminating or minimizing exposure to the virus, and we can potentially decrease the severity of this infection by giving RSV immunoglobulin to vulnerable individuals.
Decreasing exposure occurs by making sure that we frequently wash our hands. We must always wash our hands before and after encountering a new environment such as a new room, a church, a shop, or a new person and a sick person. Also, extremely important is that we avoid touching our faces with our hands.
Introducing infectious viral agents to our mucous membranes in eyes, nose, and mouth significantly increases the chances of getting sick. Finally, if we are in proximity to a person suffering from confirmed RSV infection, we should be wearing a gown, gloves, and a mask to prevent the passage of infected secretions to our body, especially face.
Vulnerable infants such as babies who were born very prematurely or ones that suffer from certain congenital heart conditions or chronic lung diseases can be protected to a certain degree from RSV infection by receiving RSV immunoglobulin.
It is still debated how useful and how cost-effective is RSV immunoglobulin; therefore, recommendations for the administration of this medication keep changing. Also, different insurance companies have different rules on who should be covered and who shouldn’t.
You can also read more about RSV prevention on the CDC website here.
What are the recommendations for the use of RSV immunoglobulin?
(Note that these recommendations change almost every year)
RSV immunoglobulin called Palivizumab is an antibody produced using DNA technology. The antibody prevents the virus from entering human cells and slows down its multiplication and proliferation. Palivizumab is believed to reduce the risks of RSV affecting the lower respiratory tract.
It may also decrease the number of hospital admissions due to the disease. At this time, we do not have any proof that this medication is capable of reducing RSV related mortality or subsequent childhood asthma.
Most experts agree that costs of RSV prophylaxis using Palivizumab exceed benefits from a small number of hospitalizations avoided even if we take under consideration only infants at higher risk for RSV complications.
Due to the above mentioned perceived low benefit from prophylaxis and high cost of therapy, insurance companies, and professional organizations developed various recommendations regarding who, when, and how many times should be treated with RSV immunoglobulin. Those recommendations often differ among different stakeholders.
If the infant qualifies for therapy with Palivizumab, the treatment should be started at the beginning of the RSV season. The medication should be given once a month as an intramuscular injection and for no more than five doses. In cases where the baby acquires infection and gets admitted to the hospital with it, prophylaxis can be stopped.
Which infants can be candidates to receive RSV immunoglobulin?
- Preterm infants born at less than 29 weeks of GA and who are younger than one year at the start of RSV season
- Preterm infants born at less than 32 weeks of gestation who developed the need for oxygen for more than 28 days and who are younger than one year at the start of the RSV season
- Babies who were born at less than 32 weeks and are still treated for chronic lung disease with medications or oxygen and are younger than two years at the start of RSV season.
- Some children with congenital heart conditions after cardiology consultation to check if they are likely to benefit from the prevention
- Diagnosis of Down Syndrome by itself is not an indication for the prophylaxis
- Diagnosis of Cystic Fibrosis itself is not an indication for the RSV prophylaxis
(Above, I gave only some examples of indications for RSV prophylaxis in infants. For a full list of recommendations, refer to CDC guidelines, AAP guidelines, Red Book, and your Health Insurance Organization. Remember that those recommendations tend to change very often.)
Are any long term consequences after RSV infection?
Most patients affected by Respiratory Syncytial Virus infections recover without any long term bad outcomes. However, there is some data to suggest that infants who had infections of lower respiratory airways such as pneumonia and bronchiolitis during the first months of their lives are prone to developing wheezing episodes later on in their life.
In Summary:
RSV is a viral infection of the respiratory tract affecting children. In some infants, particularly former preemies, it may lead to more severe conditions and require hospitalization for a few days. Those children may need to be treated with intravenous hydration and supplementary oxygen.
Very few infants will need to be placed on a ventilator. Prognosis is generally good, but every year there are some deaths reported as a result of this infection. Some babies may be candidates for medical prophylaxis using an antibody called Palivizumab.
Undoubtedly, the best approach to the prevention of RSV infections is proper hygiene and avoidance of contacts with sick children and adults.
If you want to know how to prepare for your premature baby coming home from the NICU, read my article here.
Disclaimer:
This article is only for general information purposes. It should not be viewed as medical advice. There is a small chance that information here may be inaccurate. You should always discuss all health-related matters with your doctor before making any decisions that may affect your health or health of your family members.

